Healthcare and Automation

Key Takeaways
- Healthcare is a complex and over-regulated industry which means automation will spread unevenly and result in less job losses in the short term, compared to other industries.
- Administrative tasks especially in hospitals and clinics are one of the main areas available for immediate automation.
- Additional training to use AI-supported systems will be necessary for medical personnel as well as even for patients themselves.
- There will be far less prescription errors which currently cause thousands of deaths per year in the U.S. alone.
- Surgery will be even less invasive and even more precise.
- Precision medicine (targeting the needs and profile of a specific patient) will be greatly augmented by AI-based automation.

On May 12, 2017, a the WannaCry ransomware cryptoworm began infecting machines around the world, including hospitals in the UK’s NHS. Some of them were still using the unsupported Windows XP although reportedly 98% of all infected computers worldwide were using Windows 7. The UK hospitals were paralyzed for several days. While the ransomware was sophisticated, a few upgrades and patches would have protected those hospitals.
Why hadn’t these systems been upgraded with these simple patches? The hospitals were too busy to even realize their importance.
As you read through this guide to automation in healthcare, remember this term: clinical workflows. Think of it as a series of tasks done by different healthcare workers across different work environments to deliver care – in a hospital or a clinic.
Got a new technology you want medical workers to use? It had better fit in with the workflows.
In other words, while there are lots of rapidly advancing technologies that are helping clinics and hospitals deliver care more effectively, efficiently, and with less error, the bottleneck in implementing these technologies has often been medical staff and especially administrative staff. Any new technology has to be user friendly for overworked medical staff and administrators, and not just patients, if it’s going to see wide adoption.
Make no mistake, automation in healthcare is happening and will continue to happen at an accelerating rate. The key is to see what it takes for any new technology to be successfully adopted by hospitals, clinics, and medical centers in the U.S. which will be the main focus of our article.
Or, in other words:
“Automation is good, so long as you know exactly where to put the machine.”
Eliyahu Goldratt – former Israeli Management Guru and expert on constraints (bottlenecks) in business processes
Overview of the Healthcare industry right now in the United States
Industry Snapshot
If you’re an adult (or even a teenager) living in the US, you’ll know how complex the healthcare system in America is. It’s a spiderweb of Federal and State regulations with public and private health systems co-existing in a complex network of health plans, policies, and regulations. There is no consistent, federal system coast to coast. Instead, an individual’s health plan depends on:
- Where you live (regulations vary from State to State)
- Whether you have private health or public health
- If you have private health whether you have employer-based insurance or contract directly with a private health insurance provider
- If you have employer-based insurance, whether it includes dental and vision care
- If you have public health whether it’s Medicare, Medicaid, or charity based because you have no health plan
- If you have Medicare whether you receive your coverage through a private Medicare Advantage plan
- If you have Medicaid, whether you receive your benefits through a private Managed Care organization
- What prescription drug benefits your health plan offers you, if any
And that’s just a rough sketch – I’m sure many readers can think of additional details (lots of them) that they could add. However, we’re here to focus on automation in healthcare with a U.S. focus, and only give enough detail to illustrate the many areas in healthcare ripe for increased automation.
What is clear, however, is that the shared responsibility between health providers, insurance companies, federal, state and local governments, pharmaceutical companies, and patients means the need for large scale data analysis using AI is overwhelming. How quickly the enormous array of data bases will be gathered into a workable platform or a series of platforms that are both accessible and secure, may depend on policy as much as it does on technology.
Given that caveat, however, the sooner the enormous amount of data, including Electronic Health Records (EHR), clinical trial results, and other data, can be easily accessed by medical workers and hospital and clinic administrators, the sooner it will become clear – to paraphrase Eliyahu Goldratt – where to put the machines.
Even more importantly, please remember the following as you read our article. No matter how many policy debates filled with acrimonious accusations and angry patients complaining about overworked hospitals, doctors, and health workers in general, automation is rapidly proceeding and will continue to proceed. Don’t let the policy debates distract you from that fact.
The U.S. healthcare system is world-class, innovative, unfair, discriminatory, charitable, and lifesaving. None of this precludes automation working its way through the industry. Keep your eyes on the machines to see where the future will be.
Who is this industry run by right now?
Again, this is a complex question as healthcare in America involves a network of providers and government agencies, including:
- Hospital networks (often non-profit which still charge substantially for their services),
- Medicare, Medicaid, Veteran’s Healthcare Administration, Childrens Health Insurance Program (CHIP),
- Federal and state regulators, the Centers for Disease Control and Prevention (CDC) and National Institutes for Health (NIH),
- Health insurance companies that work either with employers or with patients who purchase their health coverage directly,
- Managed care organizations and Pharmacy benefits managers,
- Pharmaceutical companies.
| Government Agencies | Multinationals | Large Businesses | |
| Hospital Networks | Generally, they are large non-profits with well over 1,000 employees although some may be smaller and operate within the U.S. | ||
| Centers for Medicare & Medicaid Services | Enormous Government Agency with over 6,000 employees that administer Medicare and Medicaid insurance programs | ||
| CDC | Large government Agency with nearly 11,000 employees in 2015, likely much higher today, post-COVID | ||
| NIH | A giant Government Agency comprised of 6 major institutions with 18,500 employees in 2021. | ||
| Health Insurance Companies | The top health insurance companies are enormous organizations with many thousands of employees but mostly provide coverage within defined regions of the U.S. – essentially dividing up healthcare by geographic zones. | ||
| Pharmaceutical Companies | The pharmaceutical industry tends to be run by large multinationals with a presence in many countries around the world. |
To see where much of the investment in automation is taking place and will continue to take place, it is helpful to detail the top insurance providers and the top health systems (hospital networks) in America.
The top 10 health insurance companies in the U.S. are as follows:
| Health Insurance Company | Market Share | Patients covered |
| Kaiser Permanente | 12.81% | 8,828,765 |
| Elevance Health (Anthem) | 7.27% | 4,670,236 |
| HCSC | 6.88% | 4,419,293 |
| United Health Group | 6.70% | 4,306,492 |
| Centene Corp. | 6.17% | 3,962,897 |
| CVS Health Corp. (Aetna) | 4.01% | 2,574,348 |
| Guide Well (Florida Blue) | 3,88% | 2,491,019 |
| Blue Cross Blue Shield of Michigan | 2.08% | 1,337,400 |
| Highmark | 1.61% | 1,035,585 |
| Blue Cross of North Carolina | 1.40% | 897,649 |
Perhaps even more importantly, the top 10 Health Systems in the U.S. are:
| Health System (Hospital Network) | Based in | Number of Hospitals |
| HCA Healthcare | Nashville, Tennessee | 182 hospitals |
| Veterans Health Administration | Washington, DC | 171 hospitals |
| CommonSpirit Health | Chicago | 140 hospitals |
| Ascencion | St. Louis | 139 hospitals |
| Trinity Health | Livonia, Michigan | 88 hospitals |
| LifePoint Health | Brentwood, Tennessee | 84 hospitals |
| Community Health Systems | Franklin, Tennessee | 79 hospitals |
| Advocate Health | Charlotte, N. Carolina | 67 hospitals |
| Tenet Healthcare | Dallas, TX | 61 hospitals |
| Christus Health | Irving, TX | 60 hospitals |
As we’ll demonstrate below, it is in hospitals where a lot of processes can be fully or at least partially automated, including:
- algorithms assisting or even replacing radiologists in spotting malignant tumors,
- AI helping to find participants for clinical trials for new medications,
- Natural Language Processing being used to analyze raw clinical notes on patients and prepare reports, or
- using robotic surgery to help surgeons perform less invasive and more precise work.
Many of these have in fact already begun.
Approximate employment numbers
| Country | Total healthcare employees | As a percentage of total workforce |
| Global | 65 million | 2.0% |
| U.S. | 18 million | 11.0% |
| China | 14 million | 1.9% |
| Canada | 2.7 million | 13.6% |
| Australia | 1.7 million | 12.6% |
| EU | 14.7 million | 7.1% |
| India | 5.76 million | 1.3% |
As far as what the future holds, the U.S. Bureau of Labor Statistics estimates that 1.9 million jobs in healthcare will become available each year in the United States over the next few years, both from new jobs being created and due to retiring healthcare professionals and workers.
Does this fit with increasing automation throughout healthcare? Or instead, are BLS statisticians old-fashioned pencil pushers out of touch with the coming wave of automation?
One possibility is that both are true, and the coming wave of automation in healthcare will mean health workers of all kinds will have to acquire new skills to deal with new technologies rather than be replaced by the tech. And more importantly, processes at hospitals and clinics will have to become more like software development. That is, more flexible and agile – meaning they will have to continually adjust their patient care to near-instantaneous feedback loops provided by AI analysis of huge databases.
Given how bureaucratic and complex healthcare is – especially in America – this will be a challenge. The OECD reports that in the United States, 45% of people working in hospitals are in administration or support staff. Think about that. Almost half of people working in a hospital (on average) in the U.S. are non-medical staff. In fact, the percentage of non-medical staff in hospitals is similar in most developed countries, according to the OECD report.
Clearly, if hospitals want to focus more on their patients and less on documentation and managing electronic records, administrative staff are ripe for AI-based automation to manage EMRs.
What is the main objective of the Healthcare industry, including the growth model, right now?
Given government regulation of healthcare even in the case of private healthcare providers, it’s all about cost savings:
- Hospital networks need to find savings by using AI to cut down on unnecessary medical services and to streamline administrative processes.
- Hospitals also need to automate those repetitive processes that can be done safely to lower costs.
- Health insurance providers want to have clear limits to what can be paid out under any health plan and are using AI – especially big data to train algorithms – to spot what they consider waste and fraud.
- Pharmaceutical companies need quickly-and-well-designed clinical trials to save time and bring their new medications to market in less time.
What is the current investment in automation in this industry?
| No investment | Low investment | Moderate investment | High investment | Full automation |
| Most tasks performed manually or with little automation | Automation limited to only a few areas or processes | Automation in wider range of areas & processes – more integrated into daily operations | Automation widely adopted & integrated into most areas & processes yielding significant improvements in productivity | Almost all tasks & processes automated with humans focused on maintenance and supervision of automated systems |
| Countries with lowest densities of health workers – darker reddish brown in map below. | Countries with relatively low densities of health workers – lighter reddish brown on the map. | Countries with mid-level densities are shown in light blue on the map below. | Countries with higher densities are shown in darker blue on the map. | No countries as of 2023. See our future timelines. |
In healthcare, it appears that there is a positive relationship between automation and the size of the healthcare workforce in any given country. This is because more developed countries have a higher percentage of people employed in healthcare, as can be seen from our employment figures above. An exception to this rule is Cuba, which has large numbers of healthcare workers but low investment in technology and automation.
Keeping this relationship in mind (more workers = more investment in automation), consider the following map:
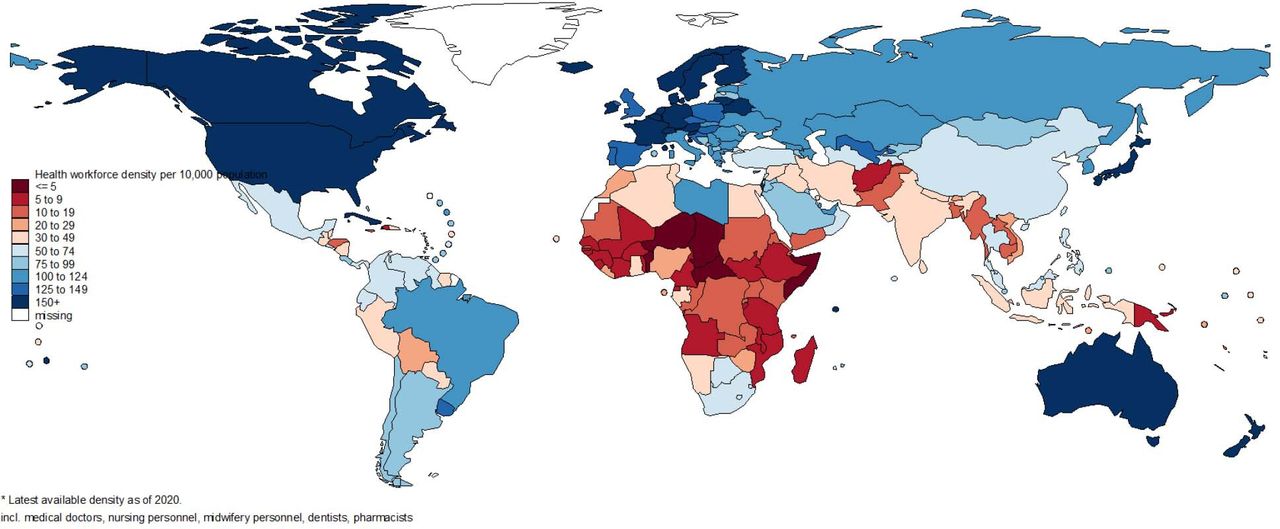
A higher density of health workers per 10,000 population is shown by darker blue. Lower density of health workers is shown by darker reddish-brown. Mid-levels are shown by lighter shades of blue or reddish-brown.
Expedited Timeline of Transformation
How will the industry start changing? What to look out for?
We have seen that automation in healthcare is currently linked to countries with large health workforces – as a percentage of their overall workforce. The billion-dollar question is whether employment will fall as automation proceeds in this industry. Most organizations related to healthcare, however, predict an increasing need for health workers as populations age around the globe and health workers retire.
Are they mistaken?
In this section, we’ll first examine what technologies will be increasingly used and then try to understand how this will affect health workers themselves.
ALGORITHMS & MEDICARE ADVANTAGE
- Health insurance companies are now using AI-based algorithms to assess a patient’s mobility and cognitive state in order to determine how long they should stay in a nursing home after an accident and/or operation. One such product is called nH Predict, created by a company called NaviHealth which is now owned by UnitedHealth Group. The product uses AI to crunch massive amounts of data and create predictive guidelines for how long patients need to stay in care facilities.
- The opportunities for this technology arose as a result of some of the compromises made in the Affordable Care Act of 2010 that gave healthcare providers under programs like Medicare Advantage a lump-sum payment up front, requiring them to find ways to control costs in order to earn a profit. An algorithm like nHPredict is an effective way to do that.
- Right now, there’s a battle between patient advocate groups and health insurance companies who work under Medicare Advantage over how flexible plans should be when managing post-acute care. However, it’s clear that algorithms like nH Predict are here to stay, even if attempts to regulate them result in their being watered down.
- Finally, a technology like nH Predict will probably create jobs – like data scientists and software engineers needed to build them, train them, and run them – more than it will kill jobs. At some point, however, it should reduce the need for administrative staff.
PREDICTING & PREVENTING COLORECTAL CANCER WITH AI
- In Singapore AI-assisted technologies have been able to identify pre-cancerous polyps more effectively, enabling them to be surgically removed before they develop into cancer.
- This is because AI-assisted technology can more accurately distinguish between pre-cancerous and non-cancerous polyps by identifying polyps that are often missed in a standard colonoscopy.
MACHINE LEARNING & PRECISION MEDICINE
- Precision medicine involves predicting what protocols are likely to be successful with a patient based on the types of possible treatments and the medical profile and clinical history of a patient.
- The technologies are developed using what is called a training dataset in a process known as supervised learning.
- Neural networks – which have existed since the 1960s and have been used in medical research for decades – can be used to assess whether a patient will develop a particular disease, for example.
- Neural networks that have layer upon layer of countless variables are used for what is called deep learning. Deep learning is being used in radiomics, defined as detecting clinically significant features in imaging data that are not visible to the human eye. Radiomics in turn is used to detect cancerous tumors and other oncology-related features in imaging data.
- It’s important to note that human observers often have difficulty understanding why a deep learning model arrives at the conclusions it does, giving rise to “black box” descriptions of the poorly understood processes. This gives rise to the possibility that in the future deep learning models will have to train their human operators – assuming human operators are still needed to interpret the results and deliver them to patients.
- Statistical Natural Language Processing (NLP) models based on deep learning neural networks, have the ability to analyze raw notes from doctor’s consultations with patients and provide reports that organize the raw data, as well as transcribe doctor’s interactions with patients.
ROBOTS & ROBOTIC PROCESS AUTOMATION (RPA)
- Surgical robots allow human surgeons to operate with greater precision providing carefully targeted incisions that are barely invasive.
- Robotics-assisted surgery is already being used in areas like gynecological surgery, prostrate surgery, and head and neck surgery.
- Robotic Process Automation – which involves computers rather than actual robots – brings together workflow processes, business rules, and integration with information systems to provide efficient, intelligent use of these systems. This can accomplish tasks like pre-authorizations, billing, updating patient records, or extracting information from fax images.
- However, the really exciting developments involve combining these aspects of automation. For example, robots can be trained using AI to increase their capacities, helping them develop AI-based artificial brains, or AI can be used to augment RPA’s abilities with image recognition.
- Key challenges with robotic-assisted surgery are training the AI algorithms on a large enough and suitable database, as well as training medical personnel how to work with an intelligent machine.
- For the time being, few predict that surgeons will be completely replaced by robotic processes which instead are seen as helping humans provide safer and more precise surgery.
DIAGNOSIS & TREATMENTS FOR CERTAIN TYPES OF CANCER
- Google is working alongside health delivery systems creating prediction models based on big data to alert clinicians of high-risk conditions in patients. Other machine-learning technologies are being developed which signal which patients are most at risk from a given condition as well as identifying which patients are most likely to respond favorably to given treatments.
- Other technologies focus on diagnosis and treatments of some types of cancer by focusing on their genetic profiles and analyzing large databases that involve lots of information on DNA and genetic variants of the cancers, an exhausting task for mere humans.
ADMINISTRATIVE WORKFLOW ASSISTANTS
- On average, doctors spend over 15 minutes per patient filling out Electronic Health Records. Ai-powered workflow optimization allows doctors to spend more time dealing with their patients.
- Using machine learning, Robotic Process Automation (RPA), and Natural Language Processing, AI can:
- Transcribe clinical data recorded during patient visits
- Give personalized responses to EHR requests
- Simplify booking of appointments
- Prioritize patients (who the doctor should see first due to urgent conditions)
- Discharge patients quickly
MACHINE LEARNING & PRESCRIPTION ERRORS
- 5 to 7 thousand patients die in the U.S. from mistakes in prescriptions every year. This in turn is often caused by flaws in Electronic Health Record (EHR) interfaces – the portals that medical professionals and support staff use to record a patient’s medical history and other relevant information, including dosage and type of medication.
- Machine learning trained on patient data compares EHR data with prescriptions and alerts doctors and nurses when a dosage or medication deviates from typical patterns.
- Additionally, machine learning can:
- Prevent drug overdosing
- Speed up electronic authorization
- Speed up review of clinical documentation for drugs that require approval
- Monitor whether patients use their medications appropriately
- The challenge is for healthcare organizations to standardize and strengthen their own databases to provide consistent data that can be safely used to train AI technology.
VIRTUAL NURSING ASSISTANTS
- Virtual nursing assistants monitor patients’ vital signs and other parameters, as well as their medications and their daily habits, to prevent the worsening of chronic conditions and to schedule necessary medical appointments.
- They can take the form of an Avatar with a chatbot to allow patients to discuss their concerns and requests, and to book an appointment. User feedback with this kind of virtual nursing assistant has been generally positive.
- Another key factor is they can provide quick and accurate answers about illnesses and medications. They can therefore be a trusted alternative to the current trend of patients using google to research their self-described symptoms, which often leads to serious mistakes by patients.
- A key challenge is ensuring robust cybersecurity for these assistants to avoid leakage of Protected Health Information (PHI). To do this, providers considering virtual nursing assistants need to:
- Build strong data protection controls
- Think about risk mitigation procedures
- Set up strong defenses against PHI leakage and malware attacks
PATIENT ENGAGEMENT
- More involvement by patients – especially trying to comply with their doctor’s recommendations in areas like weight, exercise, and diet – usually means better health outcomes. AI has the capability to help by providing message alerts and targeted content to nudge patients towards fuller engagement with their health providers. To do this requires machine learning that manages multi-channel communications to any device the patient uses.
- This idea can be further developed into what is called Choice Architecture where patients behavior is anticipated and suggestions or nudges are sent by a variety of means, based on data analysis of similar groups of patients. The data would come from a number of sources, including:
- Electronic Health Records
- Biosensors
- Smart Phones
- Smart Watches
- Automated chat interactions
The suggestions produced by this Choice Architecture technology would then be sent to patients, doctors, and nurses, or even call-center agents.
VIRTUAL REALITY & PAIN MANAGEMENT
- A company called AppliedVR has a virtual reality product, RelieVRx, that consists of a headset and software and helps manage chronic pain by helping patients through a series of pain management exercises. Providers can bill the Centers for Medicare and Medicaid Services (CMS) for AppliedVR’s device as durable medical equipment.
- The process involves what is called immersive therapeutics using virtual reality, augmented reality, and mixed reality to shift the brain’s perception of pain.
- This avoids the use of pharmaceutical products which may produce unwanted side effects.
ADMINISTRATIVE RED TAPE
This is the first real area of automation in healthcare where significant job cuts could occur much sooner than elsewhere in the system. On average, nurses in the U.S. spend 25% of their time doing paperwork to comply with policies and regulations, for example.
- Robotic processing automation (RPA) can do wonders here in areas like claims processing, medical records management, and clinical documentation, freeing up medical staff to spend time with patients.
- Chatbots have not proved very popular with patients, but refinements and younger generations of patients may change this. They may be best suited for now for simple tasks like refilling prescriptions or booking appointments with their provider.
- A more promising area mentioned above is Health Insurance companies using machine learning trained on patient data to identify fraudulent or mistaken claims, although there has been pushback from patient advocacy groups. Nevertheless, claims audits can be greatly improved by using AI as is already occurring in the industry.
What will this industry look like when automation is fully complete?
The first thing to realize is that a machine always makes the same mistake while a human makes mistakes that are more random. So, while a human can be more creative and innovative, it’s easier to correct a machine, especially in situations that require accuracy rather than creativity.
With this mind, it’s inevitable that automation will continue to spread throughout the healthcare industry. The remaining question is: what will healthcare workers’ future look like?
RM – a pioneer in education technology located in Oxford, UK has a very useful model for analyzing the stages a business or organization goes through when adapting to machine learning. The model focuses on educators marking papers/tests and shows how automation slowly takes over the process. However, it can be used to analyze any context involving machine learning automation.
There are 6 stages in the model:
- 4 with human control
- 2 final stages with partial and then fully autonomous machine learning
Here’s what their model might look like when applied to healthcare.
| HUMAN HEALTHCARE | MACHINE HEALTHCARE | ||||
| Stage 0 Human-only Healthcare | Stage 1 Process Improvements | Stage 2 Augmented Healthcare | Stage 3 Tentative Healthcare | Stage 4 Human-primed Auto-Healthcare | Stage 5 Autonomous Auto-Healthcare |
| No automation of activities | Machine learning automates and improves existing processes | Healthcare workers are first exposed to machine learning. Workers interact with AI supported functions that augment the healthcare experience. | AI assists healthcare workers, making suggestions or explaining how to perform some tasks. | AI can make decisions and do tasks based on learning with a human-built data set. | Fully automated healthcare requiring no human assistance aside from general guidelines and regulations. |
| No AI | AI has no influence on decisions made by healthcare workers | AI does not directly affect healthcare workers’ decisions | Healthcare workers are still in complete control and can validate AI suggestions or ignore them | Human priming ensures the AI retains the qualities and preferences of human healthcare workers. | AI sufficiently intelligent to make decisions based only on the guidelines given. The AI is now the only entity making decisions. |
| FULL EXTENT OF AUTOMATION ACROSS DIFFERENT AREAS OF THE HEALTHCARE INDUSTRY | |||||
| Most Emergency Room Procedures & Certain types of surgery | All other types of surgery & any process requiring a human monitor like acute post-operative care or neo-natal care, as well as radiology and pathology. | Any patient care that can be done without direct contact with healthcare workers. | All administrative tasks and all maintenance tasks and some aspects of patient care including blood tests, urine tests and other tests. | ||
| TIME FRAME FOR U.S. HEALTHCARE AUTOMATION TO REACH THE STAGES SHOWN ABOVE | |||||
| 2023 | 2023 – 2035 | By 2045 | By 2050 | By 2035 | |
Timeline – Approximately when will this industry be fully automated?
It is doubtful that – for the foreseeable future – the healthcare industry will be fully automated. As explained at the beginning, there is too much complexity and regulation by government in the U.S. and across developed countries. However, as shown in our table above, parts of healthcare can easily be fully automated within about a decade and much of healthcare should be partially or almost fully automated within less than 30 years.
Possible political and legal restraints of automation of this industry
- In December 2022, the Federal Government proposed rules that would prevent insurance companies working under Medicare Advantage from denying coverage to patients based on internal, proprietary, or external clinical criteria not found in traditional Medicare coverage policies. Whether this proposal actually becomes a regulation remains to be seen, but it shows the power of regulatory agencies have over healthcare in much of the developed world.
- Privacy concerns around leakage of Private Health Information (PHI) will drive demands for additional security measures to prevent this from happening, including attempts at restricting the use of automation in certain administrative areas.
- The difficulty even for experienced physicians in explaining how a deep-learning algorithm works will be a challenge – especially in the case of malpractice lawsuits where accountability for mistakes has to be established. Training for medical personnel and perhaps an improved understanding of these algorithms could solve the problem, but this will be a significant challenge.
- These concerns suggest that regulatory bodies will be expanded to put in place more rules and regulations (or “structures” as they like to say) to deal with automation. To what extent this will limit the spread of automation in healthcare remains to be seen.
The positive
- Less errors in medical tests and less mistaken diagnosis or missed diagnosis.
- Less prescription errors will improve patient outcomes.
- Less time spent in medical consultations because of automated paperwork
- Less paperwork for medical staff.
- Less invasive surgery (something that has already been occurring for decades now)
- Clinical studies will be set up more efficiently.
The Negative
- Patients will have less contact with humans during any medical process.
- Obtaining insurance coverage will become more demanding for borderline cases.
- Administrative and support staff will see job losses.
- Medical personnel will have to undergo training to learn to work with AI-supported systems.
- More patient engagement will be necessary to interact with new technologies which will be a challenge for older patients.
